Cell Aging – Reversed?

Scientists from the Technion have found a way to rejuvenate the aging process of the body’s immune system.
Professor Doron Melamed, principal investigator in the Richard and Kenneth Skodnek Developmental Immunology and Aging Research Laboratory, and doctoral student Reem Dowery sought to understand why the elderly population is more susceptible to severe cases of COVID-19 and why the vaccines seem to be less effective and wane faster among this population. The results of their work were published recently in the peer-reviewed, online medical journal Blood.
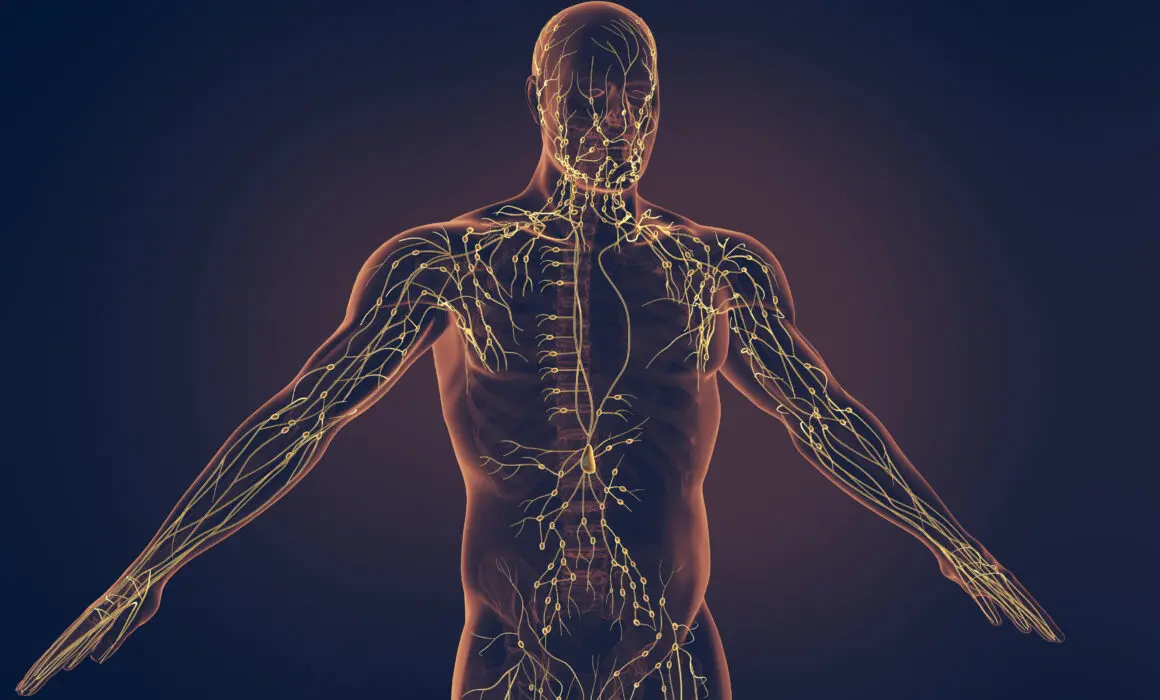
The secret begins with B cells, also known as B lymphocytes, which protect us from viruses and diseases. B cells are produced in bone marrow and then travel through the blood to lymph nodes and the spleen, where they wait for pathogens to enter and then attack them. B cells do not live long, but they are constantly being replenished by new ones sent from the bone marrow, creating what Prof. Melamed calls “homeostasis,” a state in which the total number of B cells in the bone marrow and outside remains constant.
However, B cells do not just disappear. They turn into “memory” B cells so that if the body is exposed to a previous pathogen, the individual will not get sick. That is because the immune response will be fast and robust, and it will eliminate the pathogen, often without the individual knowing he or she had been exposed to it. Unlike B cells, memory cells are long-lived. But there’s a challenge.
“Imagine you are growing into adulthood, and you become an adult and then an older person,” Prof. Melamed said. “You accumulate in your body many memory cells. You are exposed all the time to pathogens, and hence you make more and more memory cells. Because these are so long-lived, there is no room left for new B cells.”
What happens when a new pathogen, such as the coronavirus, comes along? There are no young B cells that can recognize it. That is one of the reasons why older people are more susceptible to severe COVID-19 and many other diseases. This happens because of the body’s need for homeostasis, something that Prof. Melamed’s lab discovered a decade ago. But this year, they took the discovery another step and figured out a mechanism to override the system.
“We found specific hormonal signals produced by the old B cells, the memory cells, that inhibit the bone marrow from producing new B cells,” Prof. Melamed said. “This is a huge discovery. It is like finding a needle in a haystack.”
It also means that, over time, specific drugs or treatments can be found to inhibit one of the hormones in the signaling pathway and get the bone marrow to produce new B cells.
To validate their theory, Melamed’s lab collaborated with the departments of hematology and rheumatology at Sourasky Medical Center in Tel Aviv and Rambam Health Care Campus in Haifa. As part of treatment for some medical conditions, such as lupus, lymphoma, and multiple sclerosis, patients undergo B cell depletion, meaning a significant amount of memory B cells is removed from their bodies.
Examining older patients who underwent this procedure, the group found that their immune systems rejuvenated, and their bodies could produce new B cells again. An effect similar to B cell depletion can be produced by inhibiting one of the hormones in the signaling pathway that suppresses the production of new B cells.
“Now we understand that there is some kind of conversation between compartments in the body, between how B cells are produced and what controls that,” Prof. Melamed said.
In the interim, he recommended that doctors use this knowledge to protect the elderly better, such as by instituting a vaccination program targeted just for the adult population that preempts variants with an additional shot.
“Even every three or four months, vaccinate them again and again to ensure they maintain high antibodies,” Prof. Melamed said.
He also suggested mixing vaccines, such as combining a shot of a Pfizer mRNA vaccine with an AstraZeneca booster given several months later, “which may generate better stimulation of the elderly immune system.”
At the same time, said Prof. Melamed, clinical trials would be needed to determine how to safely inhibit the hormones to find a longer-term solution, hopefully before the next pandemic.
More About
More Health & Medicine stories

New System Eases Patient Discharge Process