Promising Breakthroughs
Groundbreaking, Multidisciplinary Research Explores Radical New Frontiers in Medicine
Understanding that medicine has much to contribute toward our knowledge of engineering, and vice versa, the Technion is one of few technical institutions in the world that boasts its own medical school. Technion faculty have facilitated robust cross-disciplinary research and consistently seeded and executed bold new breakthroughs that have pushed the boundaries of medicine. Here are four exciting discoveries from our talented bench of medical researchers.
Curing Neurodegenerative Diseases
The good news: The body is capable of curing neurodegenerative diseases, including Huntington’s and ALS. The bad news: It frequently fails to recognize the problem and dispatch the right solution, known as chaperone proteins. Professor Reut Shalgi led a team of researchers to explore this erratic behavior of chaperones.
The body manufactures proteins by folding long chains of amino acids in specific ways to form three-dimensional structures. However, sometimes the folding sequence goes awry, creating protein aggregates, and laying the groundwork for neurodegenerative diseases. Chaperones usually intervene before such problems occur. They help misfolded proteins refold and prevent protein aggregation — but they sometimes don’t. Prof. Shalgi’s research explored why.
For chaperones to work, the body needs to do two things: recognize there is a problem and dispatch the right protein for the job. In the case of ALS, the cells miss the very first step — they do not even recognize there is a problem. In Huntington’s, the cells detect the problem but send the wrong proteins. As a result, the diseases progress.
Understanding what goes wrong in chaperone protein deployment could provide crucial insights for the treatment of Huntington’s and ALS. “Since the ability is there, we hope future treatments can be developed to employ the body’s own tools to cure these debilitating neurodegenerative diseases,” said Prof. Shalgi.
A Novel Way of Inhibiting Cancer Growth
Scientists have known that tumor cells grow by inviting nerve cells to infiltrate their walls, a process that feeds their growth and stimulates migration and proliferation. This led Technion researchers to explore the fundamental question: What if we could change the cancer cell–nerve cell dynamic and recruit the nerve agent to our side?
In an experiment with mice, Associate Professor Avi Schroeder and Ph.D. candidate Maya Kaduri injected nanoparticles carrying an anesthetic into the bloodstream, in the direction of the tumor. The nanoparticles were coated with a polymer that let them fly under the immune system’s radar and circulate long enough to do their job, without damaging healthy tissue. When they reached the tumor, the nanoparticles released their anesthetic into the surrounding nerve cells. The anesthetic effectively paralyzed the nerve cells and cut off communication channels that the cancer cells depend on to grow.
The team found that the method not only inhibited cancer growth, it also reduced metastasis. Given that annually, approximately 10 million people die from cancer around the world, this development is a promising achievement.
“Today, we understand that to effectively treat cancer we must not only target the cancer cells themselves but also cut them off from their supporting environment,” said Kaduri. “We believe that this treatment could significantly improve the clinical outcomes of cancer patients in the future, either as a single treatment or in combination with other therapies.”
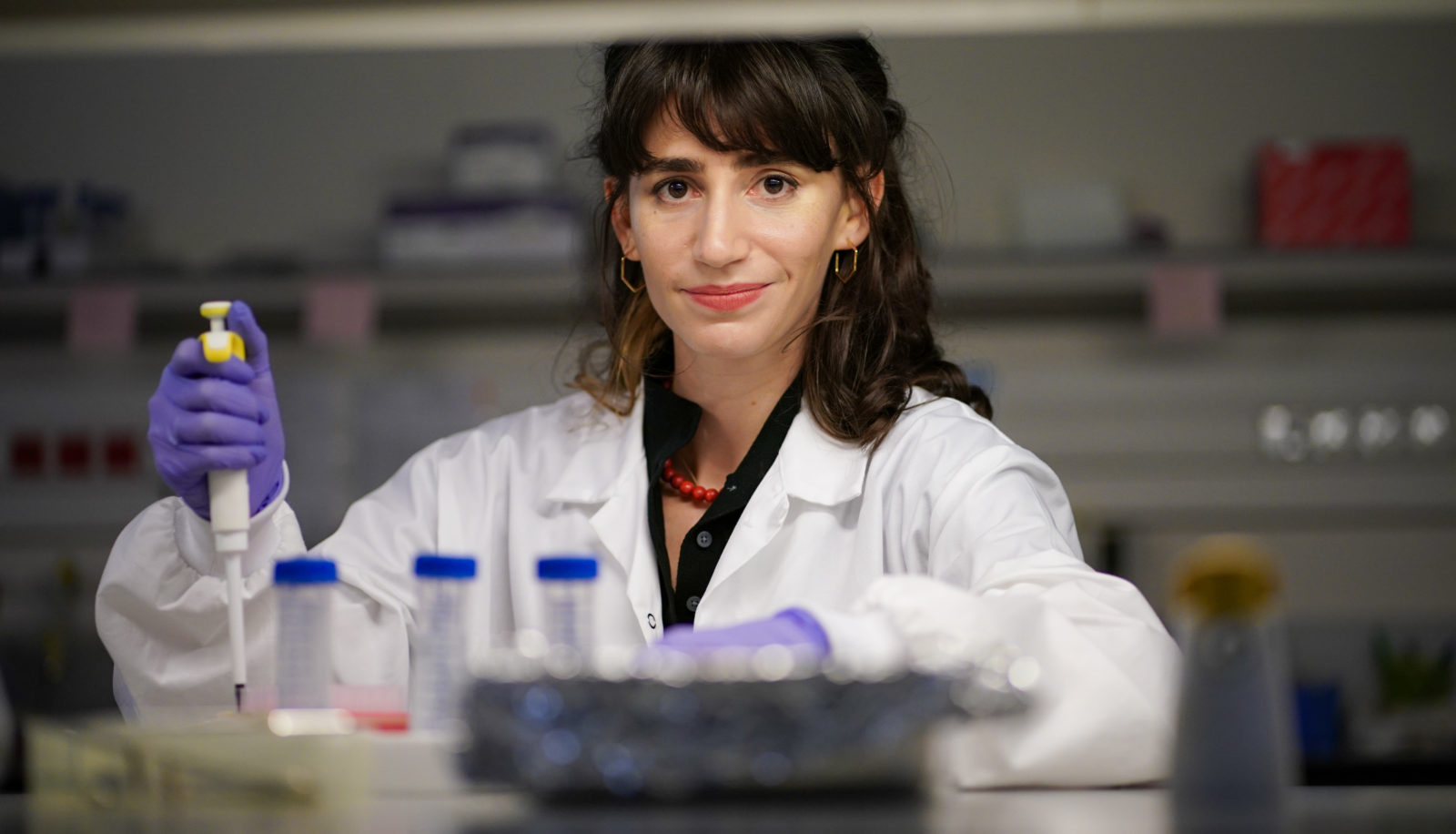
Saving the Lungs of Premature Babies
Applying a simple topical cream may go a long way toward helping premature babies — and their parents — breathe easier. Babies who are born prematurely may not have healthy lungs since the respiratory system is one of the last to mature in utero. As a result, they often require mechanical ventilators in their first days, which lack standardized methods of operation. Medical staff typically factor in the infant’s condition to adjust machine settings for the volume and flow rate of air, but these methods can be arbitrary.
Associate Professor Josué Sznitman and his team studied the complications using a 3D silicone model of premature babies’ upper respiratory tract. To truly mimic the effect of ventilation on the body, the team grew a layer of human lung cells in the model. Subjecting the artificial model to typical mechanical ventilation conditions, researchers found that forces caused by the air jet from the ventilator can create stress, inflammation, and damage in the airway cells. The team succeeded in blunting the adverse effects by applying a topical medicine usually used for asthma patients before beginning mechanical ventilation.
The findings may also help patients who require long-term mechanical ventilation — like those being treated for COVID-19 and chronic obstructive pulmonary disease (COPD). Paving the way for gentler treatment of premature babies is essential work given that 1 in 10 babies are born prematurely.
Autoimmune Diseases Might Have a New Ally: The Brain
While people have long experienced psychosomatic illness, Technion researchers have now observed exactly how the brain can make the body sick, and how to reverse it. These findings could potentially offer hope to people suffering from stress-related autoimmune diseases such as colitis, Crohn’s disease, and psoriasis.
Associate Professor Asya Rolls and M.D./Ph.D. candidate Tamar Koren induced inflammation in the colons of mice.
They were able to identify neurons in the brain that showed increased activity during the process of inflammation. Long after the mice were healthy again, the team triggered the brain neurons and the inflammation reappeared. The experiment demonstrated that the brain stored “memory traces” of the past infection that could kick-start an immune response, even without the actual presence of a disease. Testing the hypothesis in the other direction, the scientists showed that suppressing the brain cells that remembered the colitis reduced the disease in mice who were ill.
“There is an advantage to gearing up for battle when one is about to engage in the same activity again,” said Prof. Rolls. “A shorter response time would allow the body to defeat the infection faster and with less effort.”
While we need many steps to translate research from mice to humans, this finding lends deeper insight into how the brain and body work together.